COVID-19, the flu, strep, and RSV—what’s the difference? [Infographic]
The symptoms of RSV, COVID-19, strep, and the flu can have a lot of overlap. Here’s how you can identify what respiratory illness you may be dealing with, potential treatments, and when to seek care.
It’s that time of year again! Time for food, friends, and… respiratory illnesses? While testing is the only way to get a true diagnosis of what your symptoms mean, it’s good to know the differences between COVID-19, flu, strep, or RSV—and when you should seek care.
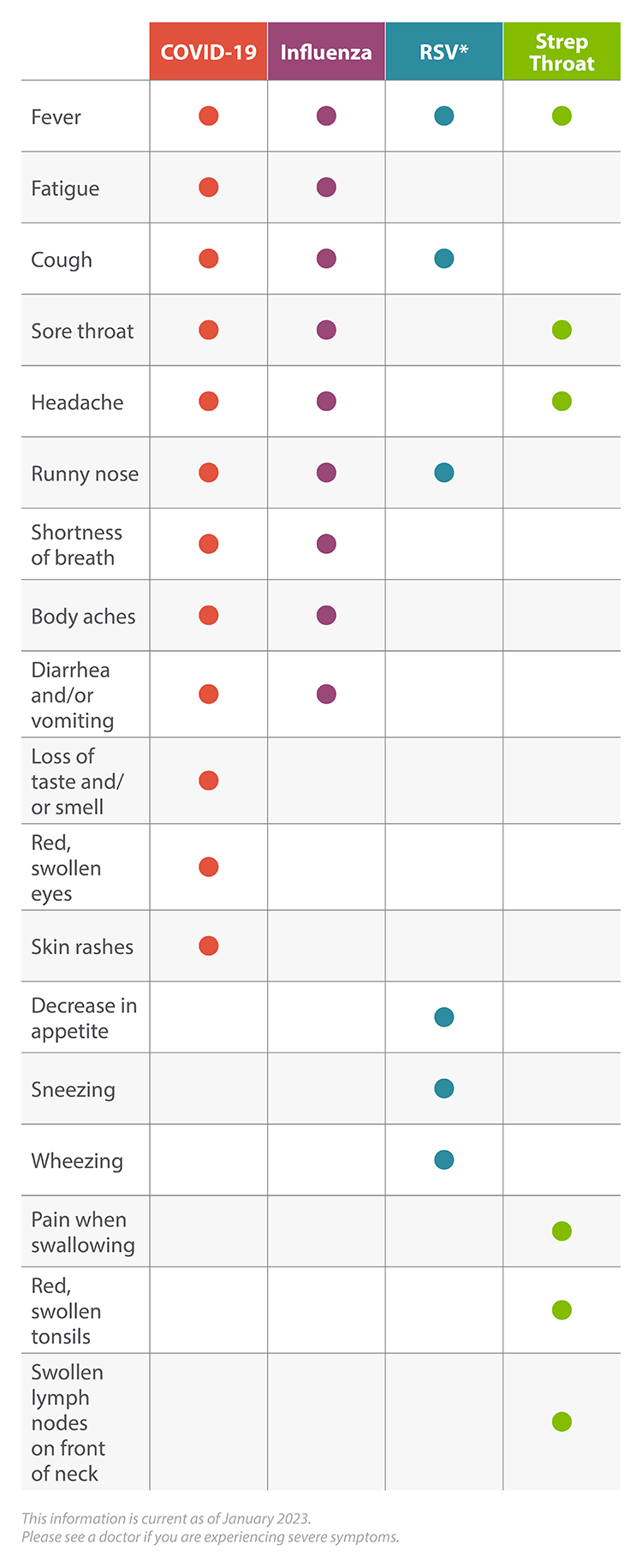
Here are the symptoms for the four major viruses this year, plus answers to some commonly asked questions.
COVID-19: Fever, fatigue, cough, sore throat, headache, runny nose, shortness of breath, body aches, diarrhea and/or vomiting, loss of taste and/or smell, red, swollen eyes, skin rashes
Influenza: Fever, fatigue, cough, sore throat, headache, runny nose, shortness of breath, body aches, diarrhea and/or vomiting
RSV: Runny nose, decrease in appetite, coughing, sneezing, fever, wheezing
*For infants with RSV, the only symptom may be irritability, decreased activity, and difficulty breathing
Strep Throat: Sore throat, pain when swallowing, fever, red, swollen tonsils, swollen lymph nodes on the front of the neck, headache
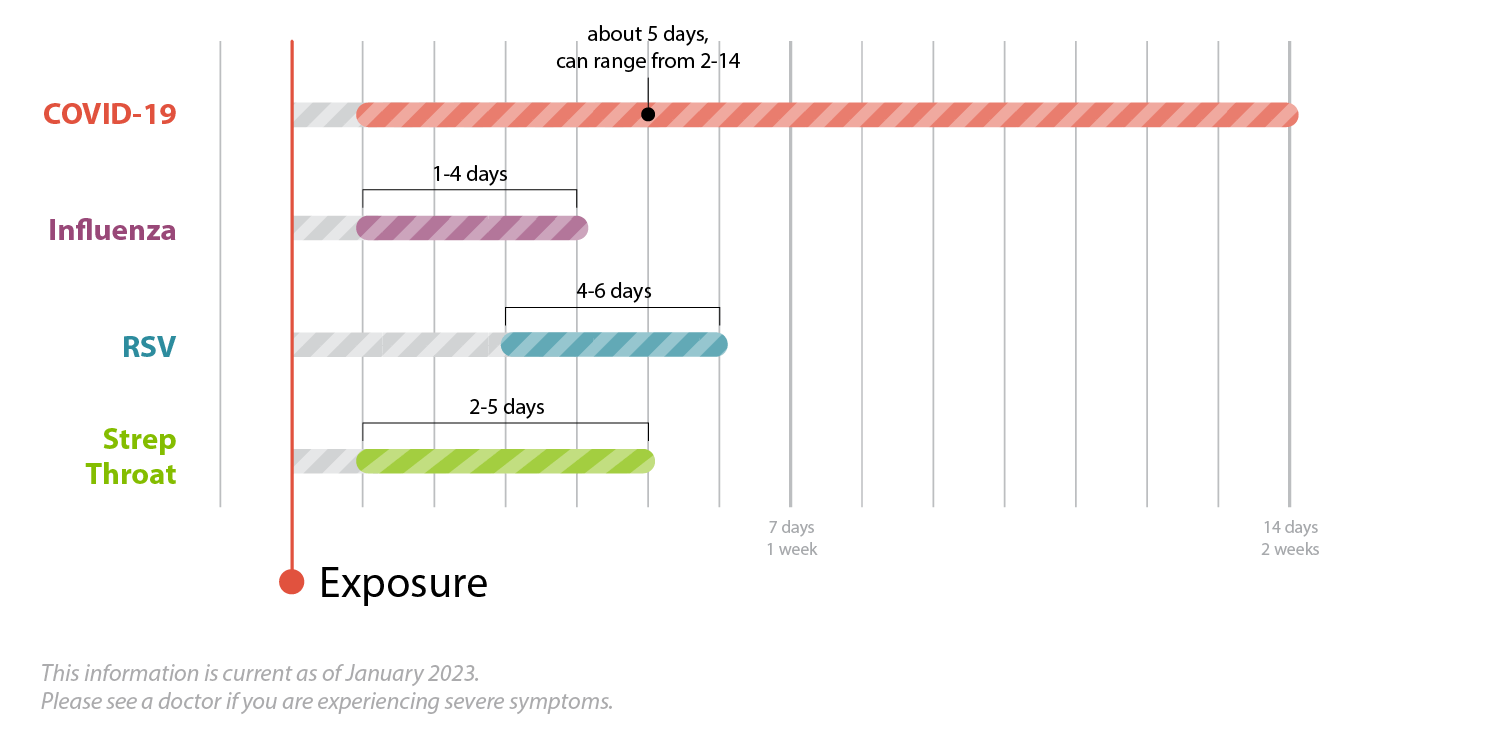
Symptom onset
COVID-19: About 5 days after exposure (can range from 2-14 days)
Influenza: 1-4 days after exposure
RSV: 4-6 days after exposure
Strep Throat: 2-5 days after exposure
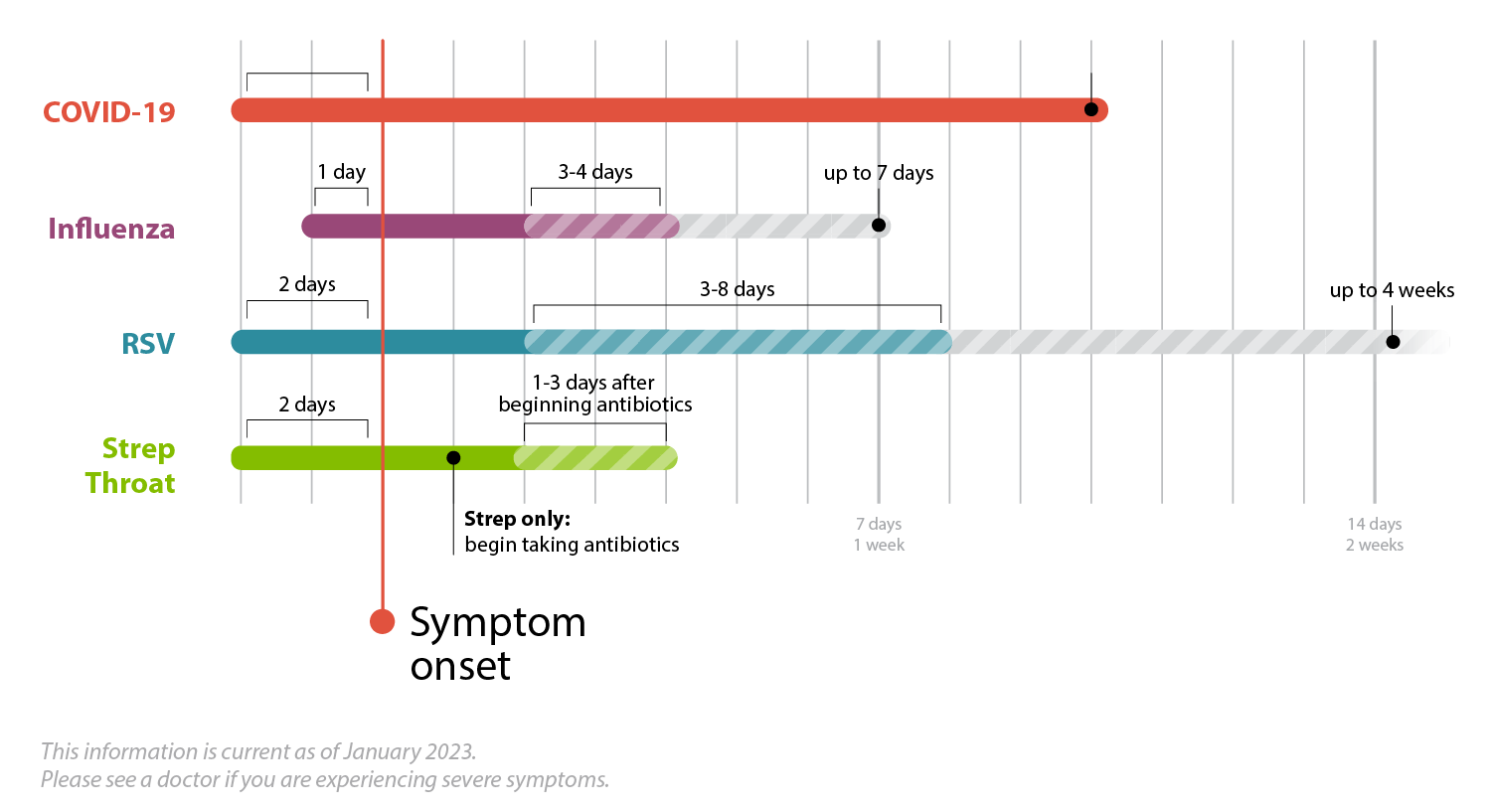
Contagious period
COVID-19: About 2 days before symptom onset and at least 10 days after symptom onset
Influenza: About 1 day before symptom onset and 3-4 days during illness (can range up to 7 days)
RSV: About 2 days before symptom onset and 3-8 days during the illness (can range up to 4 weeks)
Strep Throat: About 2 days before symptom onset, and contagious until you have taken the antibiotic for 1-3 days
High-risk populations




COVID-19: Older adults, people with underlying medical conditions, pregnant women
Influenza: Older adults, people with underlying medical conditions, pregnant women, young children
RSV: Premature infants, young children with congenital heart or chronic lung diseases, compromised immune systems, or neuromuscular disorders, adults with compromised immune systems, older adults with underlying heart or lung disease
Strep Throat: Children 5 through 15 years old, parents of school-age children , adults who are often in contact with children
COVID-19: Primarily through droplets from coughs, sneezes, or talking within about six feet of another person
Influenza: Primarily through droplets from coughs, sneezes, or talking within about six feet of another person (and possibly from contaminated surfaces)
RSV: Primarily through droplets from coughs and sneezes, direct contact, and surfaces
Strep Throat: Primarily through droplets from coughs, sneezes, and direct contact
Frequently Asked Questions
What vaccines are available for COVID-19, the flu, RSV, and strep?
COVID-19: FDA-authorized COVID-19 vaccines and boosters. Contact AFM with questions
Influenza: FDA-licensed influenza vaccines
RSV: There is no vaccine yet to prevent RSV infection, but scientists are working hard to develop one
Strep Throat: There is no vaccine to prevent strep throat
Can adults get RSV?
While it’s more common for children to contract RSV, adults can also become infected. Most healthy adults and children do not need to be hospitalized, and the infection should go away on its own. At-risk adults should see their practitioner, monitor their symptoms closely, and seek hospitalization if they experience difficulty breathing or dehydration.
I’m worried my child has RSV. When should I seek medical care?
Almost all children will get RSV at least once before they are 2 years old. For most children, RSV will have symptoms similar to a cold. But for some children, especially those considered high-risk, RSV can be severe.
Call your local AFM Urgent Care if your child is experiencing any of the following symptoms:
- Symptoms of bronchiolitis
- Dehydration (fewer than one wet diaper every eight hours)
- Pauses or difficulty breathing
- Gray or blue color to tongue, lips, or skin
- Significantly decreased activity and alertness
- Symptoms that worsen or do not improve after seven days
- A fever of 100.4F or higher for babies under 12 weeks
- A fever that repeatedly rises above 104F for a child of any age
- Poor sleep or fussiness, chest pain, ear tugging, or ear drainage
What does an RSV cough sound like?
An RSV cough sounds the same as other viral coughs. This cough will be accompanied by wheezing, runny nose, fever, decreased appetite, and fatigue.
If my child or I have RSV, should we quarantine?
No, but limit interactions until most of the symptoms have resolved. Take care not to interact with premature infants or children with chronic lung disease, weakened immune symptoms, or neuromuscular disorders, as they are at high risk for RSV.
Should I take my child to ER or Urgent care for RSV?
Consider taking your child to urgent care if they have symptoms like rapid breathing, high fever, wheezing, or severe cough. Take your child to the ER if they are struggling to breathe, have blue lips, refuse to drink, or are lethargic.
Do you need antibiotics for RSV?
Unless you develop a secondary bacterial infection, you won’t need to take antibiotics.
How long will you test positive for RSV?
It depends on the type of RSV test performed. The more sensitive the test, the longer you’ll test positive—sometimes up to several weeks. The most sensitive test is RSV RT-PCR. The most common and least sensitive test is Rapid RSV antigen testing.
Can you have the flu and COVID-19 at the same time?
Yes, it is possible to be infected with both the flu and COVID-19 at the same time. AFM works with community partners to provide COVID-19 viral PCR testing. Every person tested for the COVID-19 is also tested for influenza because of the similarities these viruses share.
Do I need to seek urgent care if I suspect that I have COVID-19, the flu, RSV, or strep?
Urgent care is an excellent place to seek care if you have symptoms of respiratory illness and want to be evaluated by a medical provider. It is also a great place to get rapid testing to determine if your respiratory symptoms are due to COVID 19, the flu, RSV, or strep and receive a clinical evaluation for potential complications of these illnesses.
What are the possible complications with COVID-19, the flu, RSV, or strep?
COVID-19
- Pneumonia
- Respiratory failure
- Fluid in lungs
- Sepsis
- Cardiac injury
- Multiple-organ failure
- Worsening of chronic conditions
- Inflammation of the heart, brain, or muscle tissues
- Secondary bacterial infections
- Blood clots
Influenza
- Pneumonia
- Respiratory failure
- Fluid in lungs
- Sepsis
- Cardiac injury
- Multiple-organ failure
- Worsening of chronic conditions
- Inflammation of the heart, brain, or muscle tissues
RSV
- Bronchiolitis
- Pneumonia
- Middle ear infection
- Asthma
Strep Throat
- Abscesses around the tonsils or in the neck
- Swollen lymph nodes in the neck
- Sinus infections
- Ear infections
- Rheumatic fever
What treatments are available for COVID-19, the flu, RSV, and Strep Throat?
COVID-19: The FDA has approved the intravenous antiviral drug Veklury (remdesivir) for adults and certain pediatric patients with COVID-19, as well as the immune modulator Olumiant (baricitinib) for certain hospitalized adults with COVID-19. They have also approved the oral drugs Paxlovid (nirmatrelvir/ritonavir) and Molnupiravir.
Influenza The FDA-approved prescription influenza antiviral drugs.
RSV: The FDA has approved the use of Synagis (palivizumab) for premature infants and young children with certain heart and lung conditions.
Strep Throat: Antibiotics like penicillin or amoxicillin
What should I do if I am experiencing symptoms associated with COVID-19, the flu, RSV, or strep?
Because respiratory viruses are contagious, it’s good to know what to do to take care of yourself and prevent the spread. Here are four tips if you’re experiencing symptoms:
1. Stay home except to seek medical care
Prevent the spread of whatever illness you may have by staying home and limiting your contact with other people. This is especially important if you have a fever.
2. See your provider
AFM has a variety of locations, hours, and visit types so you can get the care you need. Here’s how to schedule an appointment with your local AFM provider.
3. Rest, relax, and hydrate
Whether you’ve been diagnosed with a respiratory illness or simply aren’t feeling well, it’s important to get the rest you need in order to recover. Take it easy and be sure to stay hydrated. You can also call one of our primary care locations or see your provider virtually to get recommendations on over-the-counter medications that could alleviate any fever, aches, or pains.
4. Get your annual flu shot
Protect yourself and others from the flu by getting your flu shot. According to the CDC, people who get the flu vaccine are about half as likely to get sick than those who are not vaccinated. AFM offers flu shots at all of our primary and urgent care locations. Call one of our primary care locations for a same-day flu shot—free with most insurances. Or walk in to one of our urgent care clinics today.
![COVID-19, the flu, strep, and RSV—what’s the difference? [Infographic]](https://afmnoco.com/wp-content/uploads/2023/01/afm-covid-flu-rsv-strep-comparison-hero-2-1080x675.jpg)